Table of Contents
- Introduction
- Overview of ASPAC as an Emerging Market for TMS
- Importance of Mental Health Solutions in the Region
- Transcranial Magnetic Stimulation: A New Dawn for Mental Health Patients in ASPAC
- What is TMS?
- Effectiveness of TMS in Treating Mental Disorders
- Growth and Adoption of TMS in ASPAC
- Challenges and Opportunities
- Mental Health Challenges and Market Potential in the ASPAC and MENA Regions
- Prevalence of Mental Disorders in ASPAC and MENA
- Key Research Objectives
- Government Policies and Legislative Measures
- Economic Impact of Neglecting Mental Health
- TMS: A Growing Opportunity in ASPAC and MENA
- Current Market Landscape for TMS
- Barriers to TMS Adoption in the Region
- Investment Potential in the Mental Health Sector
- India’s Advancements in Mental Health Research and TMS Market Potential
- Government Initiatives and Legislative Reforms
- Expansion of Mental Health Infrastructure
- The Role of TMS in India’s Mental Health Strategy
- Impact of the COVID-19 Pandemic on Mental Health
- Rising Mental Health Issues Post-Pandemic
- Scientific Research and Trends in ASPAC
- Implications for Future Mental Health Policies
- Current Scope & Future Potential of TMS
- FDA-Approved Applications of TMS
- Ongoing Research and Future Medical Uses
- Advancements in TMS Technology
- Mental Health Crisis and the Market Potential for TMS in the ASPAC Region
- Suicide Rates and Mental Health Concerns
- Key Factors Driving TMS Adoption in ASPAC
- Challenges and Limitations in the Region
- Global Market Scenario for TMS
- TMS Expansion in Western vs. Asian Markets
- Market Potential of TMS in ASPAC and MENA
- Emerging Opportunities in China and India
- Mental Health Landscape and TMS Market Potential in Malaysia and the Philippines
- Mental Health Statistics and Government Initiatives
- The Role of TMS in Expanding Mental Health Access
- Future Prospects for TMS in These Countries
11. Mental Health Challenges and TMS Market Potential in Indonesia, Thailand, and Vietnam
- Mental Health Prevalence and Suicide Rates
- Government Policies and Legislative Frameworks
- Investment Opportunities in TMS
12. Mental Health Landscape and TMS Market Potential in Bangladesh, the Middle East, and India
- Current Mental Health Infrastructure
- Barriers to Mental Health Access
- India’s Role in Leading Mental Health Reforms
13. Conclusion: The Future of TMS in ASPAC and Emerging Markets
- Key Takeaways on Mental Health Crisis
- Opportunities for TMS Market Expansion
- Recommendations for Investors and Policymakers
14. References
Overview of ASPAC as an Emerging Market for TMS
The Asia-Pacific (ASPAC) region is rapidly emerging as a key market for Transcranial Magnetic Stimulation (TMS) due to rising mental health awareness, government policy reforms, and increasing demand for non-invasive treatments. Countries like India, China, Japan, South Korea, and Australia are experiencing a surge in depression, anxiety, and OCD, driving the need for innovative mental health solutions.
Governments across ASPAC are investing in mental health policies, insurance coverage, and awareness campaigns, while private investors and TMS device manufacturers are expanding into the region. The shortage of mental health professionals further highlights the need for scalable solutions like TMS, which allows efficient treatment with minimal human resources.
With growing acceptance, reducing stigma, and increasing accessibility, TMS is set to become a mainstream mental health treatment in ASPAC, offering a transformative solution to address the region’s mental health crisis.
Importance of Mental Health Solutions in the ASPAC Region
The Asia-Pacific (ASPAC) region is facing a growing mental health crisis, with millions suffering from untreated psychiatric disorders such as depression, anxiety, and OCD. Despite rising awareness, mental health care remains underfunded and inaccessible in many countries, leading to high suicide rates, reduced workplace productivity, and economic losses.
Key Statistics on Mental Health in ASPAC:
- India: 56 million people suffer from depression, and 38 million from anxiety disorders.
- China: Over 160 million people have mental health conditions, including 54 million with depression.
- Japan & South Korea: Among the highest suicide rates globally, with mental disorders as a major cause.
- Indonesia: Has only 0.3 psychiatrists per 100,000 people, making access to care extremely limited.
- Southeast Asia: Suicide is one of the leading causes of death among young people.
Economic and Social Impact:
- Mental disorders reduce workplace productivity, leading to billions in economic losses annually.
- Suicide rates remain high, with countries like Japan, South Korea, and India reporting significant mental health-related deaths.
- Healthcare costs are rising due to the lack of early intervention, leading to longer and more expensive treatments.
Barriers to Mental Healthcare Access:
- Shortage of mental health professionals (e.g., Indonesia: 0.3 psychiatrists per 100,000 people).
- High stigma prevents many individuals from seeking treatment.
- Limited government funding for mental health infrastructure.
- Rural areas remain underserved, while urban regions have better access to mental healthcare.
The Need for Alternative Mental Health Solutions:
- Transcranial Magnetic Stimulation (TMS): A non-invasive, FDA-approved treatment for depression, OCD, and other psychiatric disorders.
- Telemedicine & Digital Mental Health Platforms: Expanding mental health access, particularly in rural areas.
- Government-Led Initiatives: Countries like India, Australia, and Singapore are investing in mental health policies, insurance coverage, and awareness campaigns.
To effectively address the mental health crisis, ASPAC countries must:
- Expand mental health infrastructure and workforce training.
- Increase investment in innovative treatments like TMS.
- Enhance insurance coverage for mental health services.
- Continue reducing stigma through education and awareness campaigns.
By prioritizing mental health solutions, the ASPAC region can improve overall well-being, boost economic productivity, and create a more resilient healthcare system for the future.
Transcranial Magnetic Stimulation: A New Dawn for Mental Health Patients in the ASPAC Region
Transcranial Magnetic Stimulation (TMS) is emerging as a groundbreaking, non-invasive treatment option for mental health patients across the ASPAC (Asia-Pacific) region. As awareness of mental health issues grows and the demand for effective, non-pharmacological treatments increases, TMS is paving the way for a new era in mental health care.
TMS uses magnetic fields to stimulate nerve cells in the brain, particularly targeting areas associated with mood regulation and mental well-being. It has shown remarkable success in treating conditions such as Major Depressive Disorder (MDD), including treatment-resistant depression, Obsessive-Compulsive Disorder (OCD), and anxiety disorders. Unlike traditional medication-based treatments, TMS offers minimal side effects and does not require surgery, making it a promising alternative for those who have not responded well to conventional therapies.
In the ASPAC region, where mental health awareness and treatment accessibility vary significantly across countries, the introduction of TMS represents a beacon of hope for millions. Governments, healthcare institutions, and private clinics are increasingly recognizing the need for advanced mental health solutions that cater to diverse populations, including those in rural and underserved areas.
As research and clinical applications of TMS continue to expand, its integration into mainstream mental health care across ASPAC could revolutionize treatment standards, offering new possibilities for individuals struggling with mental health disorders. With continued investment, awareness campaigns, and training of medical professionals, TMS is set to redefine mental health care in the region, marking a new dawn of innovation and accessibility.
Furthermore, the growing adoption of TMS in the ASPAC region is driving advancements in mental health policies and infrastructure. Countries like Australia, Japan, and South Korea have already incorporated TMS into their healthcare systems, while emerging markets such as India, Malaysia, and Indonesia are gradually expanding access to this cutting-edge treatment. With increased research, government support, and collaborations between medical institutions, TMS has the potential to bridge the gap in mental health care, offering effective, science-backed solutions to millions who previously had limited treatment options. As the stigma surrounding mental health continues to diminish, TMS stands as a transformative force in reshaping mental health care across the ASPAC region.
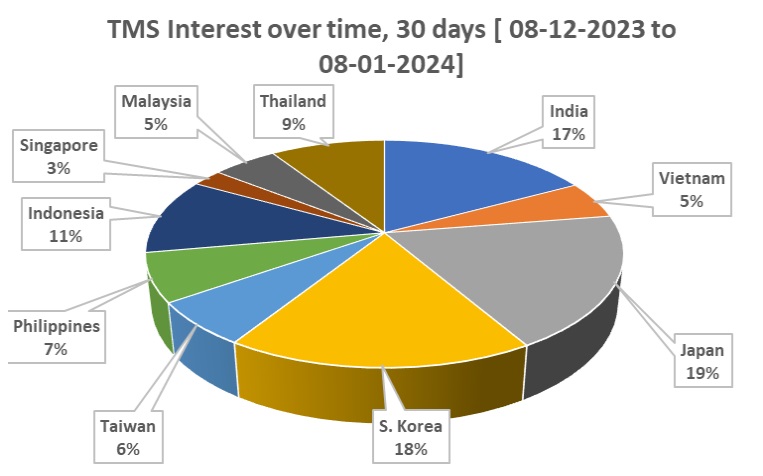
Source: Google Search Data
Mental Health Challenges and Market Potential in the ASPAC and MENA Regions
Mental health disorders remain largely underestimated in the ASPAC (Asia-Pacific) and MENA (Middle East & North Africa) regions. Conditions such as depression and anxiety have long been ignored, deprioritized, and suppressed due to deep-rooted social stigma and taboos. This neglect has led to severe consequences, including rising suicide rates, substantial economic losses, and increased financial burdens on society.
Across these regions, mental health disorders, including depression and anxiety, are widespread. However, India has emerged as the first country in ASPAC to recognize mental illness as a serious public health issue. The country has taken proactive steps to improve mental health infrastructure, allocating dedicated budgets and setting annual treatment targets to expand access to mental health care.
This article aims to provide an in-depth analysis of the current mental health landscape in Asia and MENA for stakeholders such as:
- Academics (professors and students)
- Healthcare investors (hospital owners and private sector stakeholders)
- Medical device manufacturers (particularly those involved in TMS technology)
- Government officials and policymakers
Key Research Objectives
The research focuses on several critical areas:
- Prevalence of Mental Disorders
- Analysing the percentage of the population affected by mental health conditions in various countries within Asia, MENA, and ASPAC to assess the scale and intensity of the issue.
- Market Potential and Growth Trends
- Evaluating the existing and future market opportunities in the mental health sector, including investment prospects and emerging trends.
- Impact of Social Stigma and Changing Attitudes
- Examining the role of social stigma in preventing individuals from seeking treatment and identifying how cultural perspectives are evolving in recent years.
- Economic Burden of Neglecting Mental Health
- Assessing the financial cost to national economies due to inadequate mental health policies, including losses linked to suicide, decreased productivity, and untreated mental illnesses.
- Government Policies and Legislative Measures
- Reviewing government initiatives aimed at mental health awareness, infrastructure development, and patient rights protection. This includes legislation such as Mental Wellness Acts and data protection laws similar to HIPAA in the U.S.
- Economic Indicators and Investment Insights
- Analyzing GDP, per capita income, and purchasing power parity (PPP) to determine which countries offer the most promising markets for mental health investments. This assessment is crucial for TMS manufacturers and investors in identifying viable investment destinations.
- Development of Mental Health Treatment Networks
- Evaluating administrative and political measures taken by governments to build efficient treatment delivery systems, including:
- Budget allocations for mental health programs
- Establishing helplines for anonymous patient support
- Setting up specialized mental health clinics, diagnostic centres, and hospitals with trained professionals and advanced equipment
- Evaluating administrative and political measures taken by governments to build efficient treatment delivery systems, including:
These factors highlight whether governments in the ASPAC and MENA regions acknowledge mental health as both a public health issue and a socio-economic burden—and whether they are taking tangible steps to address it.
TMS: A Growing Opportunity in ASPAC and MENA
Transcranial Magnetic Stimulation (TMS) is a breakthrough non-invasive treatment introduced in 1985. It has proven to be an effective supplementary treatment for certain mental health conditions when traditional medication and counselling fail to yield desired results.
Despite its potential, access to TMS remains limited. The majority of TMS devices are concentrated in the U.S. and Europe, meaning only 35% of the global population currently has access to this treatment. In the ASPAC region, where population density is high, the presence of TMS devices remains extremely low.
However, there is a tremendous growth potential for TMS investments in hospitals and mental health units across ASPAC and MENA. Encouragingly, many governments in these regions have started recognizing the severity of mental health challenges, especially after the COVID-19 pandemic, which significantly heightened awareness of mental health issues and their economic consequences.
As a result, several countries have begun implementing legislative reforms, such as Mental Wellness Acts and Patient Data Protection Laws (similar to HIPAA in the U.S.), to address social stigma, improve access to care, and protect patient confidentiality.
Mental health is an urgent issue in the ASPAC and MENA regions, with far-reaching implications for individuals, economies, and societies. While awareness is growing and governments are taking steps to address the problem, significant gaps remain in infrastructure, treatment access, and policy implementation.
For investors, hospital owners, policymakers, and medical technology companies, this presents both a challenge and an opportunity—to contribute to a rapidly evolving sector while addressing a critical public health need. The next decade will be crucial in determining how these regions respond to the growing mental health crisis and whether they can turn policy initiatives into lasting, impactful change.
India’s Advancements in Mental Health Research and TMS Market Potential
India has taken significant steps in addressing mental health issues, particularly by introducing the Clinical Trial Act 2019. This legislation encourages mental health research within India, aiming to attract the global research community to conduct clinical trials on the Asian population.
Moreover, Indian insurance companies have begun recognizing mental health conditions such as depression and anxiety as treatable through therapeutic interventions, marking a shift toward greater acceptance and support for mental health treatments.
Among ASPAC countries, India has demonstrated a higher level of commitment to addressing mental illnesses like Dysthymic Disorder (DD), Major Depressive Disorder (MDD), and related conditions. Recognizing the socio-economic burden posed by mental health disorders, the Indian government has taken proactive measures to build a strong mental health infrastructure.
One such initiative is Tele-MANAS, an online mental health portal designed to provide easy access to guidance and support for patients, particularly in remote areas. The details of this program will be discussed in a later section.
Expansion of Mental Health Infrastructure in India
In 2022, the Indian government established 38 specialized mental health clinics in public hospitals to provide dedicated mental health treatment. Additionally, plans are in place to equip each of these hospitals with a TMS unit, signifying India’s growing adoption of advanced mental health treatments.
The estimated demand for TMS units in public and private hospitals is projected to reach 60 to 70 units by the end of 2025. If we consider the broader ASPAC region, this demand is expected to be even higher, given the region’s large population and increasing awareness of mental health issues.
Impact of the COVID-19 Pandemic on Mental Health
The COVID-19 pandemic has exacerbated mental health issues worldwide, with increased fear and uncertainty affecting individuals’ personal and socio-economic well-being. Scientific research has linked the pandemic to the worsening of mental health disorders, including heightened levels of anxiety and depression. However, there is still a lack of controlled or longitudinal studies to establish a definitive causal relationship between the pandemic and mental health outcomes. (Reference: Research Square) [1]
Interestingly, despite the global economic impact of COVID-19 and geopolitical crises such as the Ukraine war, India’s economy has remained resilient, as evidenced by its annual growth rate, as reported by the IMF and World Bank.
Current Scope & Future Potential of TMS
With FDA approvals expanding for TMS as a treatment for various mental illnesses, confidence and acceptance of this technology are growing worldwide. As an effective non-invasive therapy, TMS is gaining interest from both patients and healthcare professionals as a viable alternative when traditional treatments such as medication and counseling do not yield the desired results.
FDA-Approved Applications of TMS
TMS has received FDA approval for treating:
- Major Depressive Disorder (MDD), including cases of treatment & medication -resistant depression
- Obsessive-Compulsive Disorder (OCD)
- Migraines
- Smoking cessation
Ongoing Research & Potential Future Applications
Research is underway to explore the effectiveness of TMS in treating additional conditions, including:
- Anxiety disorders
- Addictions
- Alzheimer’s disease
- Bipolar disorder
- Borderline personality disorder (BPD)
- Chronic pain syndromes
- Eating disorders
- Essential tremor
- Fibromyalgia
- Parkinson’s disease
- Post-Traumatic Stress Disorder (PTSD)
- Schizophrenia
- Stroke complications
- Tinnitus and auditory hallucinations
- Traumatic brain injuries (TBI)
Many of these conditions are awaiting FDA certification, and continued investment in research, technology advancements, and clinical trials will further enhance TMS protocols, improve treatment efficacy, and expand market growth. [2]
Clinical Applications & Advancements in TMS Technology
TMS has proven effective in treating various neurological and psychiatric disorders, including:
- Depressive disorders (DD, MDD)
- Anxiety disorders
- Schizophrenia
- Parkinson’s disease
- Stroke rehabilitation
- Chronic migraine pain
As research continues, new developments in coil designs, stimulation protocols, and integration with other medical technologies will further improve TMS effectiveness and broaden its clinical applications.
Types of TMS & Their Advantages
Several types of TMS technologies are available, each offering unique benefits:
- Single-pulse and paired-pulse TMS
- Repetitive TMS (rTMS)
- Navigated TMS (nTMS)
- Deep TMS (dTMS)
- Theta Burst Stimulation (TBS)
Among these, Theta Burst Stimulation (TBS) has gained attention for its ability to reduce treatment time significantly, making TMS therapy more efficient and accessible.
Future Prospects of TMS in ASPAC & Emerging Markets
Portability & Accessibility
Future advancements in TMS technology may lead to portable devices, allowing treatment to be delivered in hospital wards and even home settings. This would significantly expand patient accessibility and market growth for TMS devices.
Emerging Market Potential
While TMS adoption is growing globally, emerging markets, particularly in the ASPAC region, hold significant growth potential. As economies in these regions expand, healthcare infrastructure improves, and awareness increases, the demand for TMS technology is expected to rise sharply.
The spread of knowledge about TMS therapy and its benefits will be crucial in determining how quickly the technology is adopted. Equally important is how rapidly TMS device manufacturers expand into emerging markets.
India: A Promising Market for TMS
Among ASPAC nations, India stands out as a high-potential market for TMS, primarily due to:
- Clearly defined mental health policies and procedures
- Annual treatment targets set by the government
- Budget allocations for infrastructure development
- Initiatives for training healthcare professionals
- Legislation on patient rights and data security
With a population of 1.4 billion across 28 states and 8 union territories, India’s demand for mental health solutions, including TMS, is set to surge.
Challenges in Mental Health Data Collection in ASPAC
One of the key challenges in ASPAC is the lack of comprehensive mental health data due to factors such as:
- Limited survey mechanisms
- Social stigma and cultural taboos
- Insufficient infrastructure for mental health research
Despite these challenges, investors and stakeholders recognize the region’s vast market potential, making it an attractive destination for mental health investments.
Countries Considered for Market Analysis
The following countries are being examined for their mental health landscape and TMS adoption potential:
- China
- Singapore
- Philippines
- Indonesia
- Vietnam
- Thailand
- Bangladesh
- India
- Middle Eastern nations
India has taken significant strides in recognizing and addressing mental health issues. With progressive policies, infrastructure development, and investment in advanced treatments like TMS, the country is emerging as a leading market for mental health solutions in the ASPAC region.
The growing adoption of TMS technology, coupled with its FDA approvals and expanding research applications, presents substantial opportunities for investors, healthcare providers, and medical device manufacturers.
As awareness and accessibility improve, the future of TMS in ASPAC and MENA looks promising, offering both a solution to the mental health crisis and a lucrative market for innovation and growth.
Mental Health Crisis and the Market Potential for TMS in the ASPAC Region
More than half of the global suicides each year occur in the South-East Asia and Western Pacific regions. Suicide is one of the leading causes of death among young people and remains a major public health concern in many Asian countries. [3]
Despite the long-standing commercial use of Transcranial Magnetic Stimulation (TMS) technology in Europe and the USA for over 25 years, with FDA and CE certifications, its presence in the Asia-Pacific (ASPAC) region remains limited. Given that over 60% of the global population resides in ASPAC, and considering the rising prevalence of mental illnesses that TMS can help treat, it is critical to expand access to this proven, non-invasive treatment.
With shifting social attitudes in ASPAC, younger generations are increasingly rejecting stigma and taboos surrounding mental health. Economic development is also leading to higher disposable incomes, making quality mental health care more accessible and desirable.
Key Factors Driving TMS Adoption in ASPAC
Following factors indicate that ASPAC is an emerging and high-potential market for TMS:
- Rising Income Levels – Increased economic growth is making mental health treatments more affordable.
- Declining Social Stigma – Younger generations are more open to seeking treatment.
- Greater Awareness – Recognition that mental disorders are diagnosable and treatable is growing rapidly.
- Increased Willingness to Pay for Better Treatment – Disposable incomes are rising, enabling more people to afford quality care.
- Growing Acceptance of Mental Health Care – Societies increasingly acknowledge the urgency and importance of treating mental illness to prevent long-term social and economic burdens.
- Government Initiatives – Many ASPAC governments are launching mental health programs and increasing budget allocations.
- Insurance Support – Some countries have started including mental health treatments under insurance coverage.
- Market Demand for TMS – With limited access to alternative effective treatments, TMS presents an attractive investment opportunity.
- High Population Density – The sheer number of potential patients makes the ASPAC region an untapped but highly lucrative market.
Challenges & Limitations in the ASPAC Region
Despite the strong market potential, a key limitation remains lower per capita income compared to Western nations. However, given the high population density, a high-volume sales strategy can compensate for lower unit revenue.
For TMS manufacturers and marketers, adopting the right business model is essential to successfully penetrate the ASPAC market.
Global Market Scenario for TMS
TMS technology is not equitably available worldwide. While Europe and the USA have led the way in promotion, adoption, and research, the ASPAC region—home to 60% of the world’s population—remains underserved.
Among Asian nations, China and India are the two largest potential markets due to their sheer population size and rising demand for mental health treatments.
Market Potential of TMS in Asia and MENA Region
China: A Massive Yet Challenging Market
China has made progress in developing its mental health services, but official policies and statistics remain unclear, making market assessment challenging.
- Despite rapid economic growth, mental health has not been a national priority.
- China has the largest market potential for TMS, yet business conditions can be unpredictable.
- Reliable mental health data is scarce, as the last national psychiatric survey was conducted in 1993.
- China’s rapid urbanization has led to a dramatic increase in internal migrant workers, particularly young migrants born after 1980. This population faces significant mental health challenges due to the pressures of migration and adaptation.
Shortage of Mental Health Professionals in China
Despite the fact China has achieved tremendous success in economic development in the past but that had become instrumental for new challenges in Mental Health systems and which always assumes the low priority. [4]
- In 2014, China had only 23,000 psychiatrists—approximately 1.7 per 100,000 people.
- Many of these psychiatrists lack full qualifications, as psychiatric training remains limited in medical education.
- Mental hospitals sometimes serve political functions, detaining individuals without any actual psychiatric diagnoses.
- Psychiatrists earn less and hold lower professional status compared to other medical specialists.
Mental Health Statistics in China
A lack of government data on mental disorders makes it difficult to estimate the prevalence of specific mental disorders, as China has not conducted a national psychiatric survey since 1993. [5]
A non-governmental survey (2001–2005) of 63,000 Chinese adults revealed:
- 16% had a mood disorder, including 6% with major depressive disorder (MDD). [8]
- 13% had an anxiety disorder.
- 9% had an alcohol disorder.
- Women were more likely to have mood and anxiety disorders, while men were significantly more prone to alcohol dependence.
- Rural populations had higher rates of depression and alcohol dependence. With the continuous economic growth nearly for two decades in China, there has been a dramatic increase in internal migrant workers, from rural to urban, and there is a concern of poor mental health particularly amongst younger or “new generation” migrants who were born in 1980 or later. [6]
The Psychological Impact of China’s One-Child Policy
China’s One-Child Policy (1979–2015) created significant psychological stress, particularly among women and families who faced societal pressure and gender-based discrimination. Studies indicate that these factors have contributed to higher rates of depression and anxiety in China. [9]
Mental hospitals are also sometimes used to detain political dissidents who have no diagnosis of mental-health problems. [7]
Suicide Rates in China
Between 1995 and 1999, China’s suicide rate was approximately 23 per 100,000 people [12]. Notably:
- Depression is a leading cause of outpatient visits, making up 50% of cases at mental health clinics.
- Bipolar disorder disproportionately affects quality of life in China and other East Asian nations.
In 2007, the Chief of China’s National Centre for Mental Health, Liu Jin, estimated that approximately 50 percent of outpatient admissions were due to depression. [10],[11]
People with bipolar disorder in China and other East Asian countries experience a disproportionately greater impact on their quality of life. Since then, the rate is thought to have fallen to roughly 7 per 100,000 people, according to government data.
WHO states that the rate of suicide is thought to be three to four times higher in rural areas than in urban areas. The most common method, poisoning by pesticides, accounts for 62 percent of incidences. [12]
According to various scholars, China’s psychiatric facilities have been manipulated by government officials in order to silence political dissidents. [13], [14], [15]
In addition to misuse by the state psychiatric facilities in China are also misused by powerful private individuals who use the system to advance their personal or business ends. China’s legal system lacks an effective means of challenging involuntary detentions in psychiatric facilities. [16]
WHO estimates in their publication ‘Mental Health in China’, Depression and anxiety are the two most prevalent mental health disorders in China. Other mental health disorders include bipolar affective disorder, schizophrenia and other psychoses, dementia, intellectual disabilities, and developmental disorders including autism. [17]
One estimate shows that the number of patients suffering from mental disorders in China surpassed 160 million in 2019, ranking the country as one of the most affected by mental health-related diseases. [18]
WHO estimates 54 million people in China suffer from depression, and about 41 million suffer from anxiety disorders. [19]
At least 80% of patients suffering from depression to access treatment by 2030 (and at least 30% by 2022) according to Healthy China (HC 2030) 2019-2030 targets. [20]
The Future of TMS in the ASPAC Region
The ASPAC region represents a massive, untapped market for TMS technology. Key drivers include rising awareness, economic growth, increased acceptance of mental health care, and government initiatives.
Although China and India present the highest market potential, challenges such as lack of mental health data, stigma, and limited government prioritization remain barriers to widespread adoption.
However, as TMS technology gains regulatory approvals and becomes more affordable, its adoption in emerging economies is likely to accelerate, opening up new business opportunities for manufacturers and investors.
Expanding TMS access in ASPAC is not just a business opportunity—it is a crucial step toward improving global mental health equity.
Mental Health Scenario in Singapore
Singapore, with a population of 5.5 million (as of 2021), has a growing mental health burden. A 2018 survey by the Institute of Mental Health (IMH) found that 1 in 7 Singaporeans (785,000 people) have experienced a mental health condition in their lifetime.
The three most common mental health disorders in Singapore are:
- Major Depressive Disorder (MDD) – 343,750 cases (1 in 16 people).
- Alcohol Abuse Disorder – 230,000 cases (1 in 24 people).
- Obsessive-Compulsive Disorder (OCD) – 196,000 cases (1 in 28 people).
Additionally, 18% of Singapore’s youth are estimated to suffer from depression.
Despite being a high-income nation with ample healthcare resources, Singapore has one of the lowest rates of psychiatrists and psychologists per capita compared to similar countries.
- Singapore has 2.8 psychiatrists per 100,000 people, whereas:
- Australia has 13.5 psychiatrists per 100,000 people. [21]
- Other high-income nations have significantly higher ratios.
This shortage of mental health professionals is a major limitation in Singapore’s ability to provide adequate care for mental illness.
Key Mental Health Institutions in Singapore
- The Institute of Mental Health (IMH) – Formerly known as Woodbridge Hospital, IMH is Singapore’s only tertiary psychiatric hospital, primarily relying on medication and counselling for treatment.
- Private Neuro Hospitals – Singapore has eight private neuro hospitals that provide specialized care.
Economic Impact of Mental Health Disorders in Singapore
The economic cost of depression and anxiety symptoms in Singapore is estimated at 2.9% of GDP. Given the high prevalence of undiagnosed cases, employers and policymakers must invest in more effective mental health solutions. [22]
Mental Health Policies in Singapore
Mental Health (Care and Treatment) Act 2008 (MHCTA)
The MHCTA allows the government to detain individuals with mental health conditions who pose a danger to themselves or others.
- Detainment period:
- Up to 72 hours for initial assessment.
- Up to 12 months for extended treatment.
- Key concerns:
- The government does not track rehabilitation outcomes for detained patients.
- No amendments have been made to align the law with international human rights standards under the Convention on the Rights of Persons with Disabilities (CRPD).
The Mental Health (Care and Treatment) Act (MHCTA) grants the State the authority to detain individuals who have, or are suspected of having, mental health conditions and who may pose a risk to themselves or others. These individuals can be admitted to a designated psychiatric institution for assessment and treatment. The initial detention period can last up to 72 hours, with the possibility of extension for a maximum of 12 months, depending on the individual’s mental state.
The Institute of Mental Health (IMH) provides care based on each patient’s mental health needs and does not specifically track rehabilitation outcomes for those detained under the MHCTA.
At present, the Ministry of Health (MOH) has no plans to amend the MHCTA following Singapore’s ratification of the Convention on the Rights of Persons with Disabilities (CRPD). The existing legislation is already aligned with the requirements of Article 14 of the CRPD.
Individuals detained under the MHCTA receive the same standard of care as other patients and are treated with dignity and respect. Patients and their families are encouraged to provide feedback to IMH if they have any concerns regarding the services provided. [23]
Personal Data Protection Act (PDPA) 2012
The PDPA ensures patient confidentiality in Singapore’s healthcare system, regulating:
- Collection, usage, and disclosure of personal medical data.
- Safeguards against misuse of patient information.
- Compliance with banking and insurance regulations.
The PDPA plays a crucial role in building trust among mental health patients by protecting their data and reducing stigma-related concerns.
Objectives of the PDPA (Personal Data Protection Act, 2012)
The PDPA aims to balance the protection of individuals’ personal data with the legitimate and reasonable needs of organizations to collect, use, and disclose such data. It establishes a data protection framework to prevent misuse, ensuring the security of personal information while fostering trust in organizations that manage it.
By regulating the flow of personal data among organisations, the PDPA also aims to strengthen Singapore’s position as a trusted hub for businesses. [24]
Mental health (care and treatment) Act 2008 needs urgent revalidation depending on the current scenario.
Personal Data protection Act 2012, is a positive step forward to enhance the confidence level among the mentally ill patients to overcome the stigma attached.
Gaps in Singapore’s Mental Health System
Despite being a highly developed nation, Singapore lacks a clear roadmap for expanding mental health services.
Key challenges include:
- Low psychiatrist-to-population ratio – Mental healthcare providers are in short supply.
- Limited government intervention – Although mental health awareness is growing, policies remain underdeveloped.
- Reliance on private healthcare – The cost of mental health services in private institutions remains high, making access difficult for lower-income individuals.
The Future of Mental Healthcare in China and Singapore
China: A High-Potential but Complex Market
China represents one of the largest markets for mental health treatments, with millions suffering from depression, anxiety, and other psychiatric disorders. However, challenges such as data inconsistencies, lack of clear policies, and shortage of professionals make mental health care delivery inefficient.
Singapore: A Developed Nation with Mental Health Gaps
Despite its strong healthcare system, Singapore lacks a structured approach to mental health policy and treatment delivery. The low number of psychiatrists, high treatment costs, and limited government intervention hinder accessibility.
TMS as a Market Opportunity
Given the rising demand for non-invasive mental health treatments in both China and Singapore, TMS presents a significant market opportunity. However, to maximize its adoption, governments and private stakeholders must:
- Expand awareness campaigns to reduce stigma.
- Increase investment in training and developing mental health professionals.
- Encourage insurance coverage for TMS treatments.
- Develop policy frameworks for structured mental health care delivery.
If these gaps are addressed, China and Singapore could become key markets for TMS technology, transforming mental health care access in the ASPAC region.
Mental Health Landscape and TMS Market Potential in Malaysia and the Philippines
Mental Health in Malaysia
Prevalence and Impact
According to the Ministry of Economy, Department of Statistics, Malaysia had a total population of 32.7 million in 2022 [25]. Mental health conditions are expected to become the second-largest health concern in Malaysia after cardiovascular diseases.
The National Health and Morbidity Survey (2015), Volume II, reported alarming statistics:
- 1 in 3 Malaysian adults (29.2%) aged 16 years and above has a mental health condition—nearly triple the rate of 11.2% in 2006. A national survey by the Ministry of Health in National Health & Morbidity survey 2015, volume II, found the following: [26]
- The highest prevalence of mental disorders is in Sabah, Kelantan, Kuala Lumpur, and Sarawak.
- Among Malaysian youth (ages 13–17):
- 1 in 5 suffers from depression.
- 2 in 5 experience anxiety.
- 1 in 10 struggles with stress.
- 10.1% have attempted suicide, highlighting a critical public health concern.
Mental Health Infrastructure and Workforce
Malaysia has four psychiatric hospitals that provide mental health services:
- Hospital Bahagia Ulu Kinta (North)
- Hospital Permai Johor Bahru (South)
- Hospital Sentosa (Sarawak)
- Hospital Mesra Bukit Padang (Sabah)
However, the country faces a shortage of mental health professionals:
- There are 410 psychiatrists in both public and private sectors—a ratio of 1.27 psychiatrists per 100,000 people.
- Malaysia needs an additional 261 psychiatrists by 2025 and 493 more by 2030 to meet rising mental health demands, according to the Ministry of Health (MOH).
Growing Demand for Mental Health Services
A Malaysian Mental Health Association (MMHA) report (October 2020) highlighted that:
- Mental illness is the leading cause of disability in Malaysia.
- An estimated 2.3 million Malaysians experience mental health conditions at some point in their lives..
- The COVID-19 lockdown caused a twofold increase in mental health issues, with more Malaysians seeking counselling, primarily for stress-related concerns.
Malaysia has 10 neuro hospitals, but the current number of psychiatrists (460) remains inadequate. [27]
Key Government Initiatives
Personal Data Protection Act (PDPA) 2010
The Personal Data Protection Act (PDPA) of 2010, enforced by the Personal Data Protection Department (PDPD) under the Ministry of Communications and Multimedia Commission (MCMC), has played a vital role in reducing mental health stigma. By ensuring data privacy, the legislation encourages more people to seek treatment without fear of discrimination.
Mental Health Strategic Plan (2020–2025) & Penal Code Repeal
- The Ministry of Health’s Mental Health Strategic Plan (2020–2025) aims to improve mental health awareness, accessibility, and affordability.
The Personal Data Protection Department (PDPD), an agency under the Ministry of Communications and Multimedia Commission (MCMC), was established on May 16, 2011, following the passage of the Personal Data Protection Act 2010 (PDPA), Act 709 by Parliament. This legislative move has prompted the citizens to overcome stigma and taboo on mental health to a certain extent as the access to personal data is not easily accessible. [28]
- In a landmark move, the government repealed Section 309 of the Penal Code, which previously criminalized suicide attempts—a significant step toward mental health reform. Malaysia envisions a resilient and mentally healthy community where mental well-being is valued without stigma. The goal is to ensure timely access to comprehensive and affordable mental health care and services, fostering recovery and overall well-being.
Future Vision
The government’s goal is to create a mentally resilient society by:
- Eliminating stigma surrounding mental health.
- Providing comprehensive and affordable mental health care.
- Ensuring timely access to mental health services to promote recovery. [29]
Mental Health in the Philippines
Prevalence and Suicide Rates
With a population of approximately 111 million, the Philippines faces significant mental health challenges. According to the Department of Health (DOH):
- 3.3 million Filipinos are affected by depressive disorders.
- Suicide rates are 2.5 per 100,000 males and 1.7 per 100,000 females. [31]
- A 2020 WHO Special Initiative for Mental Health found that at least 3.6 million Filipinos have one or more mental, neurological, or substance use disorders.
- Suicide rates stand at 3.2 per 100,000 people, with higher rates among males (4.3 per 100,000) compared to females (2.0 per 100,000).
- Among Filipino youth (ages 13–17):
- 11.6% have contemplated suicide.
- 16.8% have attempted suicide, highlighting an urgent need for intervention programs. [32]
Access to Mental Health Services
- WHO reports that 8 out of every 100,000 Filipinos die by suicide, with the 15–29 age group being most vulnerable.
- An estimated 3.3 million Filipinos suffer from depression, with young people being the most at-risk group. [33]
- Only about 700 psychiatrists are currently practicing in the Philippines.
- The ratio of 0.72 psychiatrists per 100,000 people is significantly lower than Malaysia (1.27 per 100,000) and Indonesia (0.3 per 100,000).
The distribution of mental health services is highly unequal, with most psychiatrists concentrated in Metro Manila, leaving rural areas underserved.
Mental Health Legislation and Reforms
Mental Health Act (2018)
The Philippines passed its first Mental Health Act on June 21, 2018, which:
- Outlined citizens’ rights to mental healthcare.
- Ensured protections for people with mental disorders and their families.
- Mandated the integration of mental health services into primary healthcare.
Mental Health Infrastructure
- The Philippines has 10 major neuro hospitals, serving both local and international patients. [34]
- The National Center for Mental Health (NCMH), under the Department of Health (DOH), is the country’s largest mental health facility:
- 4,200 inpatient beds.
- 56,000 outpatients per year.
- Recognized as a Special Research Training Center & Hospital since 1987[35]
‘WHO’ Special Initiative for Mental Health (2021–2022)
The Philippines was selected for the WHO Director-General’s Special Initiative for Mental Health (2021), focusing on:
- Expanding access to mental health services through the Medicine Access Programme for Mental Health (MAP-MH).
- Incorporating patient voices into mental health policies and programs.
- Strengthening implementation of the Mental Health Act via training and technical guidance.
- Evaluating progress under the Philippine Council for Mental Health Strategic Plan. [36]
Challenges and Opportunities
Challenges
- Underreporting of suicide cases, often misclassified as “undetermined deaths.
- Insufficient mental health professionals, especially in rural areas.
- Restricted insurance coverage for mental health treatment.
Opportunities
- Growing awareness and government commitment to mental health reforms.
- WHO-backed programs improving treatment access.
- Expansion of telemedicine and digital mental health platforms.
Conclusion: The Future of Mental Health in Malaysia and the Philippines
Both Malaysia and the Philippines face significant mental health challenges, including rising depression and suicide rates, shortages of psychiatrists, and uneven access to treatment. However, recent government reforms, legislative changes, and WHO-backed initiatives are paving the way for improved mental health services.
TMS Market Potential
Given the high burden of mental health disorders and increasing recognition of non-invasive treatment options, TMS presents a promising market opportunity in both countries.
For Malaysia and the Philippines, the next critical steps include:
- Expanding mental health infrastructure and workforce.
- Enhancing insurance coverage for mental health treatments.
- Incorporating TMS into national mental health programs.
- Addressing stigma to encourage treatment-seeking behavior.
With government support and private sector investment, Malaysia and the Philippines could become key markets for TMS technology and mental health advancements in the ASPAC region.
Mental Health Challenges and TMS Market Potential in Indonesia, Thailand, and Vietnam
Indonesia: A Nation Facing Mental Health Challenges
Prevalence of Mental Disorders
Indonesia, with a population of approximately 274 million, faces severe mental health challenges due to deep-rooted social stigma, lack of infrastructure, and limited access to treatment. [37]
- 9 million Indonesians (3.7% of the population) suffer from depression.
- Every hour, one person in Indonesia dies by suicide, translating to a suicide rate of 2.4 per 100,000 people (World Bank Report). [38]
- Depression among the 15–24 age group stands at 6.2%, as per the Indonesia Basic Health Survey (RISKESDAS).
- 7.7% of Indonesian students exhibit mental or emotional health issues.
- Only 9.2% of young people (ages 15–24) experiencing depression seek treatment at health facilities. [39]
Mental Health Crisis Among Indonesian Youth
- 16 million people (6% of the population) aged 15 and older experience symptoms of anxiety or depression.
- 400,000 people (1.72%) live with severe mental disorders, including psychosis.
- 19% of Indonesian youth have had suicidal thoughts, and 45% have admitted to self-harm. [40]
Mental Health Infrastructure and Workforce
Indonesia, despite being the fourth most populous country in the world, faces a severe shortage of mental health professionals:
- Only 800 psychiatrists (a ratio of 0.3 per 100,000 people).
- Only 450 psychologists nationwide.
- 720 neurologists, with nearly half concentrated in Jakarta.
- 48 mental health facilities, with more than half located in just four provinces, making access a major challenge. [41]
While Yogyakarta has successfully placed psychologists in all 18 public health centres, most regions lack adequate psychiatric and neurological care. [42]
Pasung: A Harsh Reality of Mental Health Treatment
Indonesia has been under scrutiny for Pasung, the inhumane practice of chaining, restraining, or locking away people with mental health disorders.
- Though banned by law in 1977, Pasung remains prevalent in rural areas, where mental health awareness and resources are scarce.
- According to a 2013 report by the Health Ministry, 57,000 individuals with mental health conditions have been subjected to Pasung.
Essential Insights on Mental Health Investment in Indonesia
- Severe shortage of mental health professionals and services presents a significant gap.
- Young people are particularly vulnerable, with high rates of suicide, depression, and self-harm.
- Expansion of TMS treatment facilities could play a major role in addressing treatment gaps. [43]
Thailand: Rising Mental Health Concerns
Prevalence of Depression and Suicide
Thailand, with a population of approximately 70 million (as of 2021), has witnessed a growing mental health crisis:
- 1.5 million Thai youths aged 15+ suffer from depression.
- Depression and psychological disorders are increasing by 1–2% annually (Department of Mental Health). [44]
- Only 28% of people suffering from depression have access to medical treatment.
- Suicide attempts among depressed patients are 20 times higher than average, with 70% resulting in premature death.
- On average, six people attempt suicide per hour, translating to 53,000 suicide attempts per year, with approximately 4,000 fatalities annually.
Legal Framework and Government Initiatives
Mental Health Act, B.E. 2551 (2008) [46]
- Established the National Mental Health Board.
- Defined patient rights and mental health treatment protocols.
- Focused on rehabilitation and reintegration of mental health patients.
UNICEF Report (2022) on Child and Adolescent Mental Health
- 1 in 7 adolescents (ages 10–19) and 1 in 14 children (ages 5–9) suffer from mental health disorders. [47]
- UNICEF has urged the Thai government to increase mental health investments to prevent lifelong psychological harm.
UNICEF observation “Thailand must urgently increase investment in quality and timely mental health care and services for children and adolescents in order to prevent serious lifelong damage to their health, Development and future prospects” on mental health. [47]
Future Outlook for Mental Health in Thailand
- The WHO forecasts that depression will become the second leading cause of suicide worldwide among individuals aged 15–29 by 2029. [45]
- The availability of mental health services remains inadequate, requiring urgent investment in treatment infrastructure.
- TMS technology presents a potential solution, particularly for treatment-resistant depression and youth mental health disorders.
Vietnam: A Mental Health System in Transition
Prevalence of Mental Disorders
Vietnam has one of the highest burdens of mental illness in Southeast Asia.
- The prevalence of 10 common mental disorders in 2014 was 14.2%, with 2.45% classified as depressive disorders.
- The suicide rate in 2015 was 5.87 per 100,000 people.
Currently, WHO Viet Nam supports the government in developing a model of integration of mental health into general health focusing on primary healthcare. [48]
Mental Health Challenges in Vietnam
- Neuropsychiatric disorders account for 37% of disability-adjusted life years (DALYs) among adults aged 15+.
- Mental health care policies remain unclear, with limited funding and prioritization within the government sector.
- Access to mental health services is highly centralized, leaving rural areas underserved.
Mental health care in Vietnam remains hindered by unclear policies and a lack of substantial resources, particularly within the governmental sector. This initial effort to assess Vietnam’s mental health landscape has several limitations and should be viewed as a preliminary step toward developing a comprehensive profile.
Government Initiatives and WHO Support
Vietnam has begun integrating mental health into primary healthcare, with WHO support.
- WHO assists the government in integrating mental health programs into the broader healthcare system.
- Vietnam’s mental health policies are still in an early stage, requiring further development for comprehensive care.
Market Potential and Opportunities
- Vietnam presents a major opportunity for mental health investments, particularly in TMS technology and digital mental health solutions.
- There is a strong demand for treatment options beyond traditional medication, given the growing awareness of mental health disorders.
Expanding Mental Health Infrastructure in Indonesia, Thailand, and Vietnam
The mental health crisis in Indonesia, Thailand, and Vietnam is marked by high prevalence rates, inadequate infrastructure, and a shortage of mental health professionals.
Key Barriers to Mental Health Treatment in These Countries
- Severe shortage of psychiatrists and psychologists.
- Stigma and cultural taboos limiting treatment access.
- Limited government investment and unclear policies.
- High suicide rates among young people.
Opportunities for TMS Market Expansion
- Indonesia, Thailand, and Vietnam represent untapped markets for TMS due to their high demand for non-invasive mental health treatments.
- Digital mental health platforms and remote psychiatric consultations could significantly expand access to care.
- International investments in mental health infrastructure will be critical in addressing treatment gaps.
By scaling up mental health services, increasing policy support, and incorporating innovative treatments like TMS, these nations can take a transformative step toward mental health reform and improved quality of life for millions.
Given the rapidly growing mental health crisis in Southeast Asia, investment in psychiatric infrastructure, workforce expansion, and new treatment technologies like TMS will be vital for future mental healthcare developments.
With a strong policy framework, increased public awareness, and strategic funding, Indonesia, Thailand, and Vietnam can significantly improve mental healthcare access, reduce stigma, and provide effective treatment solutions for millions in need.
Mental Health Landscape and TMS Market Potential in Bangladesh, the Middle East, and India
Mental Health Challenges in Bangladesh
Current State of Mental Healthcare
Bangladesh faces significant challenges in mental healthcare, including:
- Lack of public mental health facilities.
- Shortage of skilled mental health professionals.
- Inadequate financial resources allocated to mental health services.
- Poorly implemented mental health policies.
- Widespread stigma and cultural taboos preventing access to care.
Despite a population of 162 million, the Bangladeshi government allocates only 0.44% of the total health budget to mental health services. Additionally, less than 0.11% of the population has access to free essential psychotropic medications. [49]
Prevalence of Mental Disorders
- 19% of the adult population in Bangladesh is estimated to suffer from mental disorders. The percentage of not – reported cases in Bangladesh is quite high and alarming [50], [51], [52]
- Underreporting of mental health cases remains high, making the true extent of the problem difficult to assess.
- The COVID-19 pandemic significantly worsened mental health conditions, with studies reporting:
- 57.9% experiencing depressive symptoms.
- 59.7% suffering from stress.
- 33.7% experiencing anxiety. [53]
- Among home-quarantined students, mental health distress was even more severe:
- 28.5% had stress.
- 33.3% had anxiety.
- 46.9% had depressive symptoms. [54]
Mental Health Infrastructure and Workforce
Bangladesh has one of the lowest ratios of mental health professionals in the world:
- Only 260 psychiatrists serve a population of 162 million. [56]
- Mental health services are primarily concentrated in divisional tertiary-level hospitals, making access in rural areas extremely difficult. [55]
- Limited collaboration exists between psychiatrists, psychiatric nurses, and clinical psychologists, affecting the quality of mental health care.
Key Challenges and Investment Opportunities
- Severe shortage of mental health professionals.
- Limited accessibility of treatment, especially in rural areas.
- High prevalence of undiagnosed and untreated cases.
- Potential for expansion of TMS technology to bridge treatment gaps in severe depression and anxiety disorders.
Mental Health Challenges in the Middle East
Prevalence of Mental Disorders
According to the World Health Organization (WHO), 4.4% of the global population suffered from depression in 2015. Depression is more prevalent in females (5.1%) compared to males (3.6%), with hormonal fluctuations and cultural influences cited as possible contributing factors. [57]
Studies in the Middle East and North Africa (MENA) region report depression rates ranging from 13% to 18%, with women experiencing depression at twice the rate of men. [63]
- In Egypt, depression prevalence among female adolescents is 15.3%. [58]
- In Oman, the rate among high school students is 17%. [60] , [62]
- In Saudi Arabia, 33.4% of female students suffer from depression. [61] [59]
Barriers to Mental Health Treatment
Despite the growing burden of mental illness, the gap between those needing treatment and those receiving it remains wide due to:
- Lack of education among primary healthcare providers (physicians & patients) regarding mental health. [64]
- Severe shortage of trained mental health professionals.
- Limited mental health resources in developing countries.
- Strong cultural stigma surrounding mental health issues.
| Population | Mental Stress | |
| Tunisia | 1,23,00,000 | 53% |
| Iraq | 4,35,00,000 | 49% |
| Jordan | 1,11,00,000 | 42% |
| Palaestine | 49,20,000 | 40% |
| Libya | 67,40,000 | 35% |
| Lebanon | 55,90,000 | 30% |
| Morocco | 3,71,00,000 | 29% |
| Yemen | 3,30,00,000 | 28% |
| Egypt | 10,93,00,000 | 27% |
| Algeria | 4,42,00,000 | 27% |
| Sudan | 4,57,00,000 | 22% |
Reference: Arab Barometer
India: A Leading Example in Mental Health Reform
Government Initiatives for Mental Health
With a population of 1.42 billion, India has taken significant steps to mitigate the socioeconomic burden of mental illness. Due to its extensive initiatives, a separate in-depth discussion is required (covered in Part 2).
Key Policy Highlights
- Decriminalization of suicide and suicide attempts to remove legal penalties.
- Definition of patients’ rights under the Mental Healthcare Act.
- Creation of a nationwide mental health support network, including over 50 centers.
- Launch of India’s first-ever 24×7 mental health helpline (Tele-MANAS), offering anonymous, first-line guidance by trained professionals.
Significance of India’s Mental Health Strategy
- One of the first large-scale, government-led telepsychiatry networks in Asia-Pacific (APAC).
- Breaks social stigma barriers by allowing anonymous, easily accessible mental health support.
- Demonstrates a scalable model for other developing nations in APAC and MENA regions.
Given the scope and impact of India’s mental health policies, Part 2 of this article will focus exclusively on India’s mental health landscape, infrastructure, and investment opportunities.
Conclusion: The Future of Mental Health in Bangladesh, the Middle East, and India
While Bangladesh and the Middle East continue to face severe shortages of mental health services and high levels of stigma, India has set an example through proactive policy reforms, telehealth initiatives, and expanded infrastructure.
Investment Opportunities in Mental Health and TMS Technology
- Bangladesh: High demand but limited infrastructure and professionals, making TMS expansion a potential breakthrough.
- Middle East: Increasing mental health awareness and government interest in reforms creates a strong investment market for psychiatric solutions.
- India: With a dedicated mental health policy, structured intervention programs, and insurance coverage expansion, India is emerging as a leader in mental health innovation in APAC.
By addressing barriers, increasing investment, and integrating modern psychiatric treatments such as TMS, these regions can significantly improve mental health outcomes and reduce the socioeconomic burden of untreated mental disorders.
References:
[1] India’s Covid response – Nita Radhakrishnan, Devendra Kumar Gupta – The Lancet
[2] Application of TMS, Dialogues Clin Neurosci , v.15(1); 2013 Mar ,PMC3622472, NLM
[3] Suicide and Suicide prevention in Asia, World Health Organisation
[4] VOLUME 380, ISSUE 9855, P1715-1716, NOVEMBER 17, 2012. The Lancet
[5] Mental health in China: challenges and progress, Yu-Tao Xiang, Xin Yu, Norman Sartorius, Gabor S Ungvari, Helen FK Chiu The Lancet,
[6] Mental wellbeing amongst younger and older migrant workers in comparison to their urban counterparts in Guangzhou city, China: a cross-sectional study, Jie Li, Shu-Sen Chang , Paul S F Yip, Juan Li, Lucy P Jordan, Yunge Tang, Yuantao Hao, Xingmei Huang, Ning Yang, Chaoqi Chen, Qiaomei Zeng, BMC Public Health . 2014 Dec 16;14:1280. doi: 10.1186/1471-2458-14-1280. Pub Med
[7] China wakes up to its mental-health problems, Jan 28th 2017 ,The Economist
[8] Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey, Michael R Phillips 1, Jingxuan Zhang, Qichang Shi, Zhiqiang Song, Zhijie Ding, Shutao Pang, Xianyun Li, Yali Zhang, Zhiqing Wang, Lancet 2009 Jun 13;373(9680):2041-53. doi: 10.1016/S0140-6736(09)60660-7. NLM, Pub Med
[9] Mental health penalties of having a child: findings from the China family panel studies, Xinjie Shi , Yu Shen ,Npj Ment Health Res. 2023;2(1):7. doi: 10.1038/s44184-023-00026-x. Epub 2023 May 15. Pub Med NLM
[10] Mental health in China, Wikipedia
[11] Mental health in China: challenges and progress,Yu-Tao Xiang, Xin Yu, Norman Sartorius, Gabor S Ungvari , Helen FK Chiu VOLUME 380, ISSUE 9855, P1715-1716, NOVEMBER 17, 2012, The Lancet
[12] Mental Health in China, Wikipedia
[13] Political Abuse of Psychiatry in the Soviet Union and in China: Complexities and Controversies, Richard J. Bonnie, University of Virginia School of Law, Posted: 12 Feb 2011, SSRN
[14] The Misuse of China’s Mental Hospitals, The Diplomat, By Chi Yin and Jerome A.Cohen, August 13, 2020
[15] Political psychiatry in post-Mao China and its origins in the cultural revolution, Robin J Munro, National Library of Medicine, Pub Med
[16] ina “Routinely” Uses Psychiatric Hospitals To Punish Activists: August 17 – 2022, Report, NDTV World
[17] Mental health in China, World Health Organisation
[18] Number of people with mental disorders in China from 1990 to 2019, Published by
Wenyi Zhang , Apr 14, 2022, Statistia.
[19] Creating a caring society together, World Health Organisation
[20] Health China Action plan
[21] Lifetime prevalence of major depressive disorders Singapore in 2010 and 2018, Stista
[22] Prevalence and economic burden of depression and anxiety symptoms among Singaporean adults, Parth Chodavadia, Irene Teo, Daniel Poremski, Daniel Shuen Sheng Fung & Eric Andrew Finkelstein, BMC Psychiatry volume 23, Article number: 104 (2023)
Published: 14 February 2023
[23] MENTAL HEALTH (CARE AND TREATMENT) ACT, Ministry of Health, Singapore
[24] Personal Data Protection Act 2012, Singapore,
[25] Population, The World Bank
[26] National Health & Morbidity Survey 2015
[27] Mental illness a big issue in Malaysia, Muhammad Yusry, 12-10-2022, The Sun Daily
[28] Personal Data Protection Act 2010 (PDPA) of Act 709, MyGovernment. Ministry of Communications and Multimedia Commission (MCMC), Malaysia
[29] National Strategic Plan for Mental Health 2020 – 2025, Ministry of health, Malaysia
[30] World Population Prospects 2022, Department of Economic and Social Affairs, population Division, United Nations
[31] Department of Health
[32] The 2022 National Mental Health Summit Aims to Lift the Spirits of Filipinos, Hello Doctor
[33] 6 Common Misconceptions About Depression, Hello Doctor
[34] Neurology Centres in Philippines, health-tourism.com
[35] National Centre for Mental Health(NCMH), Department of Health, Republic of Philippines.
[36] Key achievements in 2021-2022, WHO Special Initiative for Mental Health,WHO
[37] The World Bank
[38] Suicide mortality rate (per 100,000 population) – Indonesia, World Health Organization, Global Health Observatory Data Repository ( apps.who.int/ghodata ), The World Bank,
[39] Determinants of Depression in Indonesian Youth, Indri Yunita Suryaputri, Rofingatul Mubasyiroh, Sri Idaiani, and Lely Indrawati National Institute of Health Research and Development . Indonesia Basic Health Survey (RISKESDAS) 2018. Jakarta: National Institute of Health Research and Development; 2019. (Indonesian) [Google Scholar]
[40] YouGov
[41] The Jakarta Post
[42] Resources and organization of Neurology care in South East Asia, Niphon POUNGVARIN, Department of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand, Neurology Asia 2007; 12 : 41 – 46, NEUROLOGY PRACTICE IN ASIA
[43] What if…pasung were ended in Indonesia, United Nations sustainable development group
[44] The World Bank
[45] 1.5 million Thai youths are suffering from depression, numbers rising, February 2023, Thai PBS world.
[46] Mental Health Act, Thailand, WHO
[47] Alarming poor mental health trend among children and adolescents in Thailand requires urgent investment in services, 31 August 2022, UNICEF, Thailand
[48] Mental health in Viet Nam, WHO
[49] The current state of mental healthcare in Bangladesh, Pub Med Central, National Library of Medicine
[50] Islam A, Biswas T. Mental health and the health system in Bangladesh: situation analysis of a neglected domain. Am J Psychiatry Neurosci 2015; 3(4): 57–62 [Google Scholar]
[51] National Institute of Mental Health. National Mental Health Survey of Bangladesh 2018–19: Provisional Fact Sheet. NIMH, 2019. (https://www.who.int/docs/default-source/searo/bangladesh/pdf-reports/cat-2/nimh-fact-sheet-5-11-19.pdf?sfvrsn=3e62d4b0_2 [cited 16 Dec 2020]). [Google Scholar]
[52] Mental disorders in Bangladesh: a systematic review, Mohammad Didar Hossain, Helal Uddin Ahmed, Waziul Alam Chowdhury, Louis Wilhelmus Niessen, and Dewan Shamsul Alam, Pub Med Central, NLM
[53] The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study, Md Hasan Al Banna , Abu Sayeed , Satyajit Kundu , Enryka Christopher , M Tasdik Hasan, Musammet Rasheda Begum , Tapos Kormoker , Shekh Tanjina Islam Dola , Md Mehedi Hassan , Sukanta Chowdhury , Md Shafiqul Islam Khan , Pub Med, NLM
[54] The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study, Abid Hasan Khan,a Mst. Sadia Sultana, Sahadat Hossain, M. Tasdik Hasan, Helal Uddin Ahmed, and Md. Tajuddin Sikder, J Affect Disord 2020; 277: 121–8. [PMC free article] [PubMed] [Google Scholar]
[55] Pathways to care of patients with mental health problems in Bangladesh, Nazmun Nahar Nuri,1 Malabika Sarker,2 Helal Uddin Ahmed,3 Mohammad Didar Hossain,4 Claudia Beiersmann,1 and Albrecht Jahn, Int J Ment Health Syst 2018; 12: 39. [PMC free article] [PubMed] [Google Scholar]
[56] Bangladesh: WHO Special Initiative for Mental Health Situational Assessment, Global Mental Health, University of Washington
[57] Depression and Other Common Mental Disorders, Global Health Estimates, WHO
[58] Clinical characteristics of depression among adolescent females: a cross-sectional study, Afaf H Khalil, Menan A Rabie, Mohamed F Abd-El-Aziz, Tarek A Abdou, Amany H El-Rasheed, and Walaa M Sabry, Clinical characteristics of depression among adolescent females: a cross-sectional study. Child Adolesc Psychiatry Ment Health 2010. Oct;4:26. 10.1186/1753-2000-4-26 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[59] Prevalence, symptomatology, and risk factors for depression among high school students in Saudi Arabia, Abdel-Rahman A Asal 1, Moataz M Abdel-Fattah,
[60] Depressive symptoms among high school adolescents in Oman, M Afifi 1, A Al Riyami, M Morsi, H Al Kharusil, East Mediterr Health J 2006;12(Suppl 2):S126-S137. [PubMed] [Google Scholar]
[61] Silent Epidemic of Depression in Women in the Middle East and North Africa Region: Emerging tribulation or fallacy, Liyam Eloul , Aamal Ambusaidi, Samir Al-Adawi, Sultan Qaboos Univ Med J. 2009 Apr;9(1):5-15. Epub 2009 Mar 16.[Pub Med]
[62] Prevalence of Depressive Symptoms among University Students in Oman, Zakiya Al-Busaidi, Kamlesh Bhargava, Aida Al-Ismaily, Hadia Al-Lawati, Rahma Al-Kindi, Mohammad Al-Shafaee, Abdullah Al-Maniri, Prevalence of depressive symptoms among university students in Oman. Oman Med J 2011. Jul;26(4):235-239. 10.5001/omj.2011.58 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[63] Depression: Prevalence and Associated Risk Factors in the United Arab Emirates Hira Abdul Razzak,* Alya Harbi, and Shaima Ahli, Oman Med J. 2019 Jul; 34(4): 274–282. doi: 10.5001/omj.2019.56[PubMed]
[64] Major depressive disorder, mental health care, and the use of guidelines in the Middle East Oğuz Karamustafalioğlu Comparative Study, J Clin Psychiatry, . 2010:71 Suppl E1:e07. doi: 10.4088/JCP.9058se1c.07gry. [Pubmed]
Debasis Chaudhuri